Grand Valley Local Schools Activity and Rest-Break Guidelines for Extreme Heat

Preseason
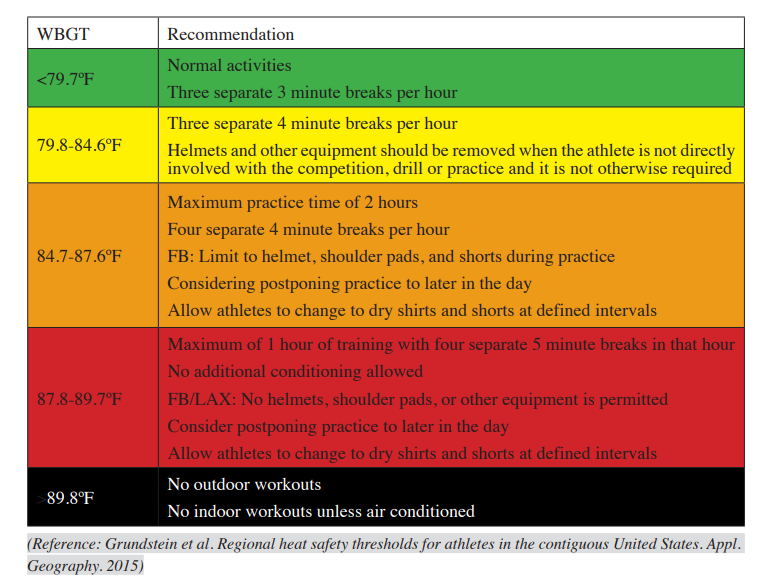
Understanding the environmental conditions is critical to our preparation. We can prevent potential problems by following the OHSAA preseason heat acclimatization guidelines for organized sports in hot and humid weather conditions. Additionally, following adaptable guidelines based on the type of activity and the wet bulb globe temperature (WBGT) is just as important, and these are included in the OHSAA guidelines.
In stressful environmental conditions (see Figure 1), particularly during the first 2–3 weeks of preseason practice and scrimmages, activity should be delayed or rescheduled or the practice session shortened to reduce the risk to participants. Particular attention should be given to practice drills involving high-intensity activity and full protective equipment worn by players, as these factors may exacerbate the body's heat stress.
Turf
Synthetic turf can reach temperatures 40-70 degrees hotter than the surrounding air during scorching temperatures. It has been recorded at temperatures ranging from 120-180 degrees Fahrenheit, which significantly increases the risk of heat-related illness (dehydration, heat stress, or heat stroke), especially in children, because their bodies are less adaptable to regulating internal body temperature (Position Statement on the Use of Artificial Turf Surfaces, 2023).
Wet Bulb Globe Temperature
As responsible Athletic Trainers and Coaches, it's crucial to regularly test the air with a wet bulb globe and temperature index (WBGT index). This index, indicated in Figure 1, combines the effects of temperature, humidity, radiant heat, and airflow and should be monitored every 30 minutes during practice to adjust the intensity of practice accordingly. If the index exceeds 89.8°, outdoor workouts should be avoided, and indoor practice should be air-conditioned. Just below that, football practices can limit the wearing of equipment. Remember, your vigilance in this matter is vital to ensuring the safety of your students and preventing heat-related illnesses. While using a physical WBGT measuring device is strongly recommended for a more accurate measure of the designated location, the Zelus app can be a good resource for athletic trainers and coaches (Sports Medicine, 2023).
Figure 1
Wet Bulb Globe Temperature Guidelines
OHSAA Guidelines
https://ohsaaweb.blob.core.windows.net/files/BulletinBoard/20230822AdministratorUpdate.pdf
Click on the hyperlink under the Heat Acclimatization and Exertional Heat Illness Prevention section. Information is on Page 5 of 7 for the Sports Medicine document.
Guidelines for hydration and rest breaks
Rest breaks should involve unlimited hydration intake (water or electrolyte drinks) and rest without activity.
Helmets will be removed during rest breaks.
The site for rest time should be a "cooling zone" and not in direct sunlight (if possible) when the WBGT reading is more significant than 86F:
Preventative strategies for cooling:
Consider using ice towels or sponges and spray bottles filled with ice water, which should be available in the "cooling zone" to aid the cooling process.
Cold water immersion tubs must be available for practices to benefit any player showing early signs of heat illness.
Communication with Athletes
It is essential to inform athletes that there are several factors they can do to help mitigate dehydration and heat-related illness:
· Adequate sleep
· Hydrate before, during, and after the activity.
· Consume hydrating foods- fruits and vegetables.
· Weight checks before and after practice to identify how much fluid needs to be replaced.
· Salty sweaters need to replace sodium. Sports drinks and salty foods are the best way to replenish lost sodium.
· Avoid participation if sick. Athletes currently or recently ill may be at greater risk for exertional heat illness because of fever, dehydration, or medications (decongestants or antidiarrheal agents) (Casa et al., 2015).
· Medications that adversely affect thermoregulation include stimulants (pre-workout), antihistamines, anticholinergics (Tylenol PM), and antipsychotics. Adherence to the acclimation period is important for these athletes.
· Avoid wearing clothing that is dark, bulky, and nonbreathable material.
· Even in similar workout conditions, athletes with higher body fat percentages can dehydrate and overheat faster than those with lower percentages.
References
Casa, D. J., DeMartini, J. K., Bergeron, M. F., Csillan, D., Eichner, E., Lopez, R. M., Ferrara, M. S., Miller, K. C., O'Connor, F., Sawka, M. N., & Yeargin, S. W. (2015). National athletic trainers' association position statement: Exertional heat illnesses. Journal of Athletic Training, 50(9), 986–1000. https://doi.org/10.4085/1062-6050-50.9.07
Position statement on the use of artificial turf surfaces. (2023, November 30). Children's Environmental Health Center Department of Environmental Medicine and Public Health. Retrieved June 20, 2024, from https://mountsinaiexposomics.org/position-statement-on-the-use-of-artificial-turf-surfaces/
Sports medicine. (2023, August 1). Ohio High School Athletic Association. Retrieved June 20, 2024, from https://ohsaaweb.blob.core.windows.net/files/BulletinBoard/20230822AdministratorUpdate.pdf
Article by Denise Fisher, Certified and Licensed Athletic Trainer for University Hospitals
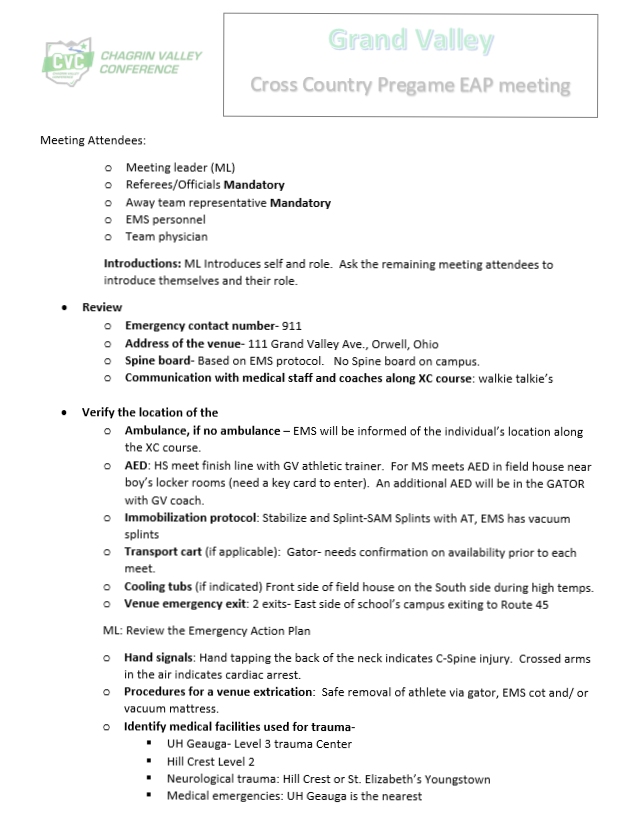
AEDin3 Challenge
The AEDin3 challenge, a groundbreaking initiative by University Hospitals, showcases an individual's ability to swiftly retrieve the AED, apply pads, and administer the first shock within 3 minutes. This challenge is not just about raising awareness, but about empowering you to bridge potential gaps in your Emergency Action Plan (EAP). It's about being prepared, whether it's understanding the need for a key card to enter the building or simply knowing the location of the nearest AED to the emergency.
Our commitment to the 'Anyone Can Save a Life' EAP extends to the AEDin3 Challenge, where we stress the importance of accessing an AED within 3 minutes. In the previous fall season, we made a significant discovery: student-athletes must be familiar with the locations and appearances of AEDs. This revelation underscores the necessity of planning, learning, and practicing emergency action plans with our student-athletes.
In addition to practicing the EAP and AEDin3 Challenge with the student-athletes, the coaches and I took part in an AEDin3 program created by Dr. Robert Flannery so that Grand Valley High School could apply for free AEDs. Dr. Flannery of University Hospitals recognized that many schools may not have AEDs accessible to student-athletes within 3 minutes during practices and sporting events. It's important to note that when an AED is delivered within 3-5 min to increase the survival rate. Every minute there is a delay, the survival rate drops by 10%. As the coaches and I practiced the AEDin3 Challenge (Spring of 2023) at different locations on Grand Valley's campus, we noted some shortfalls where an AED was further than 3 minutes away. The shortfalls occurred at various places on the cross-country course, the far end of the football practice field, and the community park in Orwell, where the soccer team practices and occasionally competes. Due to the shortfalls, Grand Valley qualified for three free AEDs. We have received two free AEDs so far, thanks to the AEDin3 Challenge and the coach's support. Frank Hall, athletic director, will decide how the two AEDs will be available: permanent wall location or portable AED with coaches.
We extend our heartfelt gratitude to Dr. Flannery and our esteemed donors and partners, the Cleveland Browns, MTKYN Foundation, Kaulig Companies, and Stryker Medical Devices, for their unwavering support of the AEDin3 program. Your contributions have not only made a significant difference in our emergency preparedness but also underscored the importance of community collaboration in ensuring the safety of our student-athletes.
15 Northeast Ohio Schools Receive the First Cardiac Defibrillators as Part of UH AEDin3 Program
Article by Denise Fisher, Certified and Licensed Athletic Trainer for University Hospitals

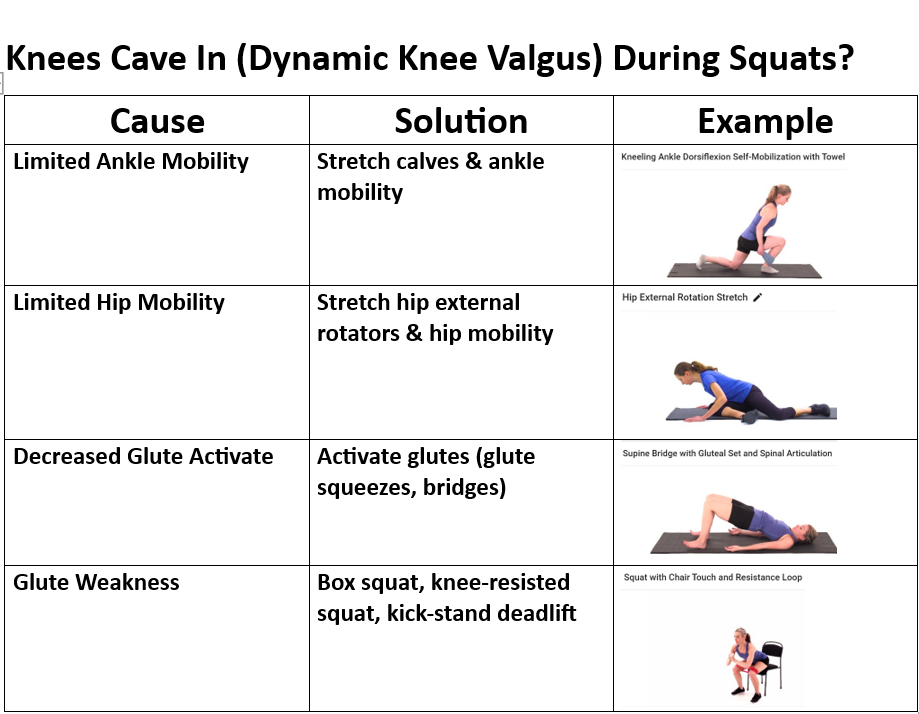
Dynamic Knee Valgus

Feet Turned Out Compensation

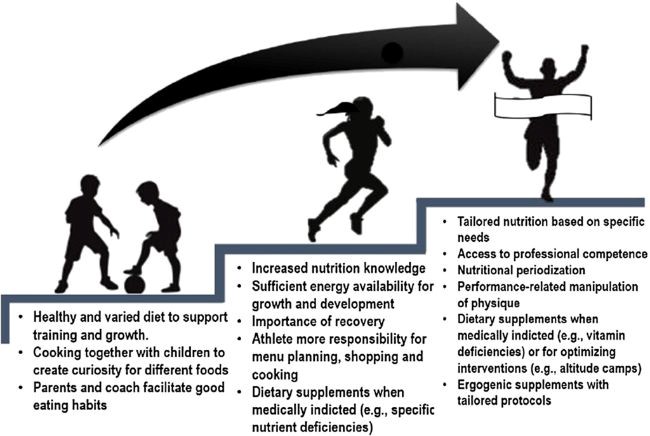
The implementation and commitment to a corrective exercise program would provide a way to offset the negative impacts on our society before the development of medical conditions. Nowadays, chronic physical inactivity in youths will exhibit habitual nonfunctional living characteristics that transpire to poor postural adaptations from their sedentary lifestyle (Fahmy, 2022), leading to high incidences of obesity, poor motor skills, and musculoskeletal disorder weakness (Liao et al., 2019). Over time poor postural adaptations will lead to musculoskeletal dysfunctions from imbalances in muscle recruitment and length between muscles that stabilize joints and muscles that mobilize joints (Comerford & Mottram, 2001). Youths may feel discouraged from traditional physical activity in the presence of a musculoskeletal dysfunction because it may not feel good to exercise, or they lack confidence and motivation, thus retreating to their sedentary lifestyle. A corrective exercise program is a safe and individualized program that identifies neuromusculoskeletal dysfunction, followed by developing an action plan and integrative exercise techniques (Fahmy, 2022). A corrective exercise program will also address the youth's environment and goals, which are essential to the program's success and the continued support of adopting a positive and healthy lifestyle (Fahmy, 2022).
Walker et al. (2018) medical report identified physical inactivity in youths as an exercise deficit disorder. The medical report examined a three-tiered strategy for preventing pediatric physical inactivity by improving the quality of life and decreasing morbidity and economic burden (Walker et al., 2018). The first tiered strategy is tertiary prevention, providing treatment for health complications from an existing disease (Walker et al., 2018). Tertiary care is the current health care model for the USA; however, in the past, before the twentieth century, the health care model focused on preventing diseases (Walker et al., 2018).
The second and third-tiered strategies are elements discussed in corrective exercise programs: early treatment and immunization against exercise deficit disorder (Walker et al., 2018). Early treatment and immunization of this disorder begin with engaging youths lacking physical activity (Walker et al., 2018). When early physical activity is promoted, youths will demonstrate improved health parameters (Walker et al., 2018). According to Walker et al. (2018), identifying and treating muscle strength and motor skills deficiencies are necessary for developing a solid foundation to carry through to later stages of development (Walker et al., 2018). A corrective exercise program would aim to address these deficiencies through the corrective exercise continuum objectives (Fahmy, 2022).
In conclusion, corrective exercise programs are valuable to this population's health and well-being. The benefits to society are considerable by applying safe and effective means of improving one's overall health and well-being from exercise.
If you are a parent of a child (athlete or non-athlete) at Grand Valley MS and HS (ages 12-18) and are interested in a free Corrective Exercise Consult, please contact me at denise.fisher@grandvalley.school. The free consult will include health history, movement analysis, education on findings of the movement analysis, and 1st phase of the corrective exercise plan. The consult generally takes about 45-60 minutes. Please note that a medical clearance may be required depending on the discoveries in the health history.
Article by Denise Fisher 6/14/2023
Certified and Licensed Athletic Trainer
Corrective Exercise Specialist
References
Comerford, M., & Mottram, S. (2001). Movement and stability dysfunction – contemporary developments. Manual Therapy, 6(1), 15–26. https://doi.org/10.1054/math.2000.0388
Fahmy, R. (Ed.). (2022). NASM Essentials of corrective exercise training (2nd ed.). Jones & Bartlett Learning.
Liao, T., Li, L., & Wang, Y. (2019). Effects of functional strength training program on movement quality and fitness performance among girls aged 12–13 years. Journal of Strength and Conditioning Research, 33(6), 1534–1541. https://doi.org/10.1519/jsc.0000000000002190
National center for chronic disease prevention and health promotion. (2022, April 27). CDC Centers for disease control and prevention. Retrieved May 12, 2022, from https://www.cdc.gov/chronicdisease/resources/publications/factsheets/physical-activity.htm
Walker, G., Stracciolini, A., Faigenbaum, A. D., & Myer, G. D. (2018). Physical inactivity in youth. ACSM's Health & Fitness Journal, 22(2), 42–46. https://doi.org/10.1249/fit.0000000000000370

Six Pack Abs
What is the best exercise for the core?
There are many excellent exercises that strengthen the abdominal muscles; however, I feel this can be seen as a controversial topic because there is so much misinformation out there, especially for the public. I admit that I used to only strengthen my abdominal muscles with full sit-ups, Roman chair leg lifts, and crunches when I was younger. It wasn’t until I went through yoga instructor training in my early 20s that I learned better ways to strengthen my abdominal muscles. However, I do feel the above exercises have a place in strength and conditioning programs, but I don’t think they are as optimal as I once thought. Brookbush (2016) did deflate my belief when he explained there is no such thing as the lower abdominals. It makes sense because you typically can not separate the action into upper or lower contractions when you tighten or draw in your abdomen. This goes back to knowing and understanding your anatomy well. Brookbush (2016) explained this based on studies that looked at the movement and stabilization of the spine, hips, and pelvis, noting that the rectus abdominis is recruited as one muscle unit. There is one caveat to the rectus abdominis as a one-unit muscle; the stomach roll in belly dancing is noted in one study to result in deliberate and separate recruitment of the upper and lower rectus abdominis muscles (Brookbush, 2016).
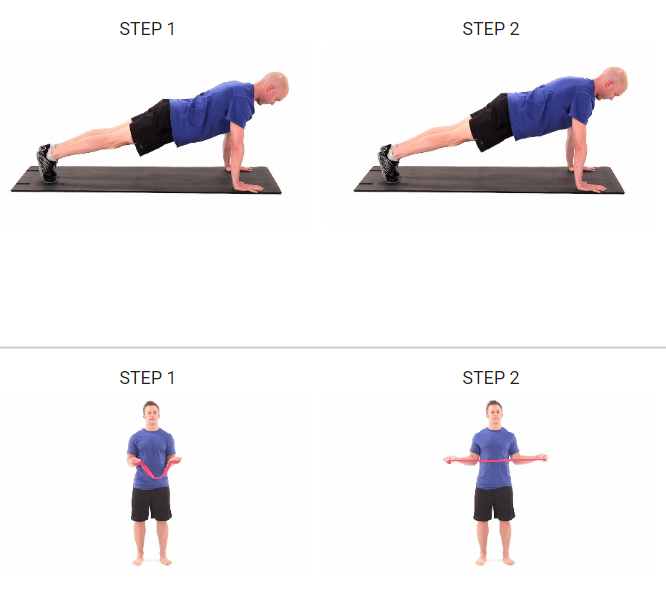
It is hard for me to identify one specific exercise that best strengthens the abdominal muscles because additional factors like physical ability, balance, mobility, and age need to be considered. Since I work with high school athletes, I must be cautious about my exercise selection because they may lack the strength and stability to perform certain abdominal exercises correctly. The exercise I have selected as the best abdominal exercise is the plank. This selection has several reasons: easy to modify, progressional, and can be done with or without equipment. I also like the plank because it is a foundational exercise that works the entire body and helps athletes transition safely to Olympic lifts by understanding core activation. The research by Snarr & Esco (2014) looked at the variations in rectus abdominis, external obliques, and erector spinae raw muscular activity and the percentage of a maximum voluntary contraction between a traditional plank and a plank with instability devices. The study used electromyography (EMG) to analyze maximum voluntary contraction (MVC) and electromyographic activity of the rectus abdominis, external obliques, and lumbosacral erector spinae. The subjects were instructed on the five different plank exercises: regular plank on forearms, plank with elbows and forearms on the Swiss ball (EB), plank with feet on the Swiss ball (FB), plank with elbows in TRX suspension trainer (ET), and plank with feet in TRX suspension trainer (FT). The research findings were interesting and very informative, which identified significantly greater EMG activity of the analyzed musculature when planks were performed with the Swiss ball or TRX suspension trainer. The ET produced the highest mean raw and %MVC for the rectus abdominis activation. The external obliques had the most increased EMG activity for both raw and %MVC with the FB. For the erector spinae, the highest raw EMG recording was with both EB and ET, and the highest %MVC was in the ET plank. This doesn’t mean planks with instability devices are superior to regular plank exercise. The traditional plank provides sufficient abdominal musculature activation to increase strength and stability (Snarr & Esco, 2014). The variation of the EMG results of the three muscles during planks with instability devices is explained by changes in the distance between the center of mass and the location of the instability device. The authors also considered the difference in EMG data between the Swiss ball and the TRX suspension trainer due to the differences in degrees of freedom.
To conclude, I consider the plank one of the best abdominal exercises because it can be modified and advanced for different skill levels. The plank also includes a total body muscle activation approach from the head to the toes allowing the individual to be consciously aware of their body alignment and isometric muscle contractions during the exercises.
Article by Denise Fisher 4/18/2023
References
Brookbush, B. (2016). Human movement science & functional anatomy of the: rectus abdominis (and pyramidalis). Brookbush institute human movement science. Retrieved December 6, 2021, from https://brookbushinstitute.com/course/rectus-abdominis-pyramidalis
Snarr, R. L., & Esco, M. R. (2014). Electromyographical comparison of plank variations performed with and without instability devices. Journal of Strength and Conditioning Research, 28(11), 3298–3305. https://doi.org/10.1519/jsc.0000000000000521
Overhead Baseball Pitch: Mechanics and Compensations that Lead to Injury
The overhead baseball pitch is an incredible demonstration of the power transmitted through the kinetic chain, generated in the lower extremity and transferred through the upper extremity (Chalmers et al., 2017). Specifically looking at the upper extremity, the overhead baseball pitch is an open kinetic chain movement (Findley & Brown, 1999). The open kinetic chain (OCK) movement does not have a fixed distal segment, enabling free movement that is not fixed to an object (Prokopy et al., 2008). It's important to note that the OKC movements can be associated with closed chain movements, which is demonstrated in the overhand baseball pitch when the forces are generated in the lower extremity before transferring up the kinetic chain to the upper extremity (Findley & Brown, 1999).
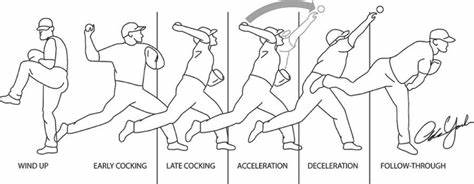
To identify the common compensations seen during the overhead pitch, one must have a general understanding of the pitching phases and how they help one to analyze muscle activity and joint actions occurring within each phase. Researchers who study the overhead pitch will use specific tools to measure kinetic, kinematics, and electromyography (EMG) during each pitch phase, allowing them to understand better what muscles are active during the phases (Escamilla & Andrews, 2009). The six phases that describe the pitching motion are wind-up, stride, arm cocking, arm acceleration, arm deceleration, and follow-through (Chalmers et al., 2017).
During the wind-up phase, the pitcher puts himself in a balanced position, which is critical for preparing force generation. Hands are together at the chest, and the lead leg is raised (Chalmers et al., 2017). Injuries are low during this phase; however, as noted by Seroyer et al. (2020), if the pitcher alters his center of gravity by initiating the movement prematurely, the force generated through the kinetic chain will be altered, resulting in significant stress at the glenohumeral and elbow joint to propel the ball forward at top speed.

The stride phase initiates the arm cocking position to generate ball velocity. The lead foot makes ground contact on the mound with the hip and knee extending while the pelvis rotates to face the batter on the home plate (Chalmers et al., 2017). During this phase, shortened stride length compensates for poor hip mobility from flexibility restrictions in the hamstring of the lead leg and stance leg hip flexors or rotators (Calabrese, 2013). Another compensation to consider is an abnormal placement of the stride foot due to decreased hip mobility, which is noted as the excessive closed foot contact position (Christoffer et al., 2019). A standard stride foot placement should be facing toward the home plate (Calabrese, 2013). The compensation occurs when the lead leg hip has overactive internal rotators and the stance foot has overactive external rotators (Calabrese, 2013). The excessive closed foot contact position will limit the lead leg and pelvis from transmitting the force to the pitching arm, which leads to timing errors and loss of proper sequence of the body and the pitching arm, causing more stress on the anterior shoulder, scapular stabilizers, and medial elbow (Christoffer et al., 2019; Calabrese, 2013). A study by Albiero et al. looked at the hip active range of motion (AROM) and pitching biomechanics during a fastball pitch in adolescent baseball pitchers. The authors hypothesized that poor active hip range of motion would decrease the energy transfer through the kinetic chain, causing subpar pitching mechanics and injury to the pitcher. The study involved twenty-one healthy adolescent baseball pitchers. The pitchers were tested by a single session that included a detailed clinical and biomechanical analysis using specialized cameras and markers. The study occurred during preseason baseball when the pitchers were already pitching twice weekly. The results indicated five significant relationships between pitching biomechanics and hip AROM flexibility. The findings confirmed the importance of having optimal hip AROM to complete normal pitching biomechanics through the kinetic chain aiding in pitch velocity and decreasing injury up the kinetic chain.

The arm cocking phase begins when the lead foot contacts the ground and finishes with maximal shoulder external rotation of the pitching arm (Calabrese, 2013). Late in this phase, significant injury can occur to the pitching arm because shoulder internal rotational torque and elbow valgus torque are at their peak (Chalmers et al., 2017). The repetitive loading leads to injuries of the superior labral anterior-posterior (SLAP) and ulnar collateral ligament (Chalmers et al., 2017). Pitchers that compensate with exaggerated shoulder horizontal abduction to increase ball velocity are at risk for anterior translation of the humeral head, which will produce internal impingement during the end of the cocking phase (Itami et al., 2018). The most common overactive muscles in the cocking phase are the teres minor, infraspinatus, and middle and posterior deltoids. The underactive scapular muscles are the upper and lower trapezius and serratus anterior muscles. The overactive and underactive muscles described above create imbalances in the pitching arm that can also be observed when the elbow is positioned below the shoulder's height during the end of the cocking phase (Calabrese, 2013).

The acceleration phase starts when the shoulder is maximally externally rotated, followed by the change to internal rotation, the extension of the elbow, and flexion of the wrist (Chalmers et al., 2017). During this phase, compensations are noted for different levels of pitchers. For example, it's not uncommon for youth and amateur pitchers to demonstrate weakness in scapular muscles and overactivity of the biceps and rotator cuff (RTC) muscles resulting in overuse injuries (Calabrese, 2013; Christoffer et al., 2019). In all levels of pitchers, maintaining stabilization of the scapula is critical for reducing the risk of shoulder impingement, RTC muscle strains, and biceps strains (Calabrese, 2013). However, according to Gowan et al. (1987, as cited in Escamilla & Andrews, 2009), professional baseball pitchers demonstrated better coordination of their kinetic chain segments, resulting in less glenohumeral instability minimizing stress to the RTC musculature and biceps.
The arm deceleration phase is the most violent in the baseball pitch because of the large forces generated at the shoulder complex to slow down the pitching arm momentum (Seroyer et al., 2010). The phase begins when the ball is released from the hand ending in maximal internal rotation of the shoulder (Escamilla & Andrews, 2009). This phase differs from the other phases because of the high compressive forces required to decelerate the arm to avoid shoulder distraction (Escamilla & Andrews, 2009). The posterior muscles are eccentrically contracting to maintain the humeral head's optimal position, while scapular muscles stabilize to reduce the forces on the RTC muscles and biceps (Calabrese, 2013). Due to the high compressive forces in the shoulder, the muscles and static stabilizers are very susceptible to overload, which is seen when a pitcher demonstrates fatigue within the kinetic chain (Itami et al., 2018). The overload will lead to scapular dyskinesia resulting in compensations at the shoulder or elbow (Itami et al., 2018). Glenohumeral internal rotation deficit is an example of a commonly discussed compensation at the shoulder from posterior capsule tightness, underactive scapular upward rotators, and retractors (Itami et al., 2018).

The last phase of the overhead baseball pitch is the follow-through. During this phase, the pitching arm moves in horizontal adduction and internal rotation as the body moves forward (Calabrese, 2013). Due to the decrease in joint loading, fewer injuries are attributed to this phase (Seroyer et al., 2010).

The best early prevention strategies to avoid future compensations noted during the overhead baseball pitch are learning the proper pitching mechanics in the beginning stages (Fortenbaugh et al., 2009) and having a balanced strength and mobilization program for the shoulder complex, trunk, and lower extremities. Another essential prevention strategy is to avoid training overuse and pitching fatigue. Fortenbaugh et al. research identified the importance of combining pitch count and kinematics/ kinetics to identify pitcher fatigue during the pitching motion more effectively. Since muscular fatigue is attributed to a high pitch count, the effects are seen later as imbalances within the shoulder and scapular muscles (Itami et al., 2018).
In closing, the overhead baseball pitch is a complex motion requiring the entire kinetic chain to work from the ground up in a systematic way to avoid injury and fatigue. In my opinion, the pitcher should be recommended to start with a strong foundation and optimal joint mobility in the upper and lower extremities and spine before learning the overhead pitching technique. Once the process is mastered, pitch volume should be determined based on the performance quality and age. Strength and endurance training programs should include open and closed kinetic chain exercises to gain the maximum benefits from both types of training. Lastly, encouraging youth athletes to avoid specialization early in their sporting careers will help decrease the risk of compensation, injuries, and burnout from year-round training.
Watch Drew Storen's pitching mechanics: Click on the link below.
Drew Storen pitching mechanics in slow motion 1000 FPS
Article by Denise Fisher 4/5/2023
References
Albiero, M. L., Kokott, W., Dziuk, C., & Cross, J. A. (2021). Relationships between hip flexibility and pitching biomechanics in adolescent baseball pitchers. Journal of Athletic Training. https://doi.org/10.4085/1062-6050-0103.21
Calabrese, G. J. (2013). Invited clinical commentary pitching mechanics, revisited. The International Journal of Sports Physical Therapy, 8(5), 660.
Chalmers, P. N., Wimmer, M. A., Verma, N. N., Cole, B. J., Romeo, A. A., Cvetanovich, G. L., & Pearl, M. L. (2017). The relationship between pitching mechanics and injury: A review of current concepts. Sports Health: A Multidisciplinary Approach, 9(3), 216–221. Retrieved October 15, 2021, from https://doi.org/10.1177/1941738116686545
Christoffer, D. J., Melugin, H. P., & Cherny, C. E. (2019). A clinician’s guide to analysis of the pitching motion. Current Reviews in Musculoskeletal Medicine, 12(2), 98–104. https://doi.org/10.1007/s12178-019-09556-4
Escamilla, R. F., & Andrews, J. R. (2009). Shoulder muscle recruitment patterns and related biomechanics during upper extremity sports. Sports Medicine, 39(7), 569–590. https://doi.org/10.2165/00007256-200939070-00004
Findley, B. W., & Brown, L. (1999). Open-versus closed-kinetic chain exercise. Strength and Conditioning Journal, 21(4), 39. Retrieved October 15, 2021, from https://doi.org/10.1519/00126548-199908000-00008
Fortenbaugh, D., Fleisig, G. S., & Andrews, J. R. (2009). Baseball pitching biomechanics in relation to injury risk and performance. Sports Health: A Multidisciplinary Approach, 1(4), 314–320. https://doi.org/10.1177/1941738109338546
Itami, Y., Mihata, T., McGarry, M. H., Lin, C. C., Patel, N. A., Kantor, A., Neo, M., & Lee, T. Q. (2018). Effect of increased scapular internal rotation on glenohumeral external rotation and elbow valgus load in the late cocking phase of throwing motion. The American Journal of Sports Medicine, 46(13), 3182–3188. https://doi.org/10.1177/0363546518800267
Seroyer, S. T., Nho, S. J., Bach, B. R., Bush-Joseph, C. A., Nicholson, G. P., & Romeo, A. A. (2010). The kinetic chain in overhand pitching: Its potential role for performance enhancement and injury prevention. Sports Health: A Multidisciplinary Approach, 2(2), 135–146. https://doi.org/10.1177/1941738110362656
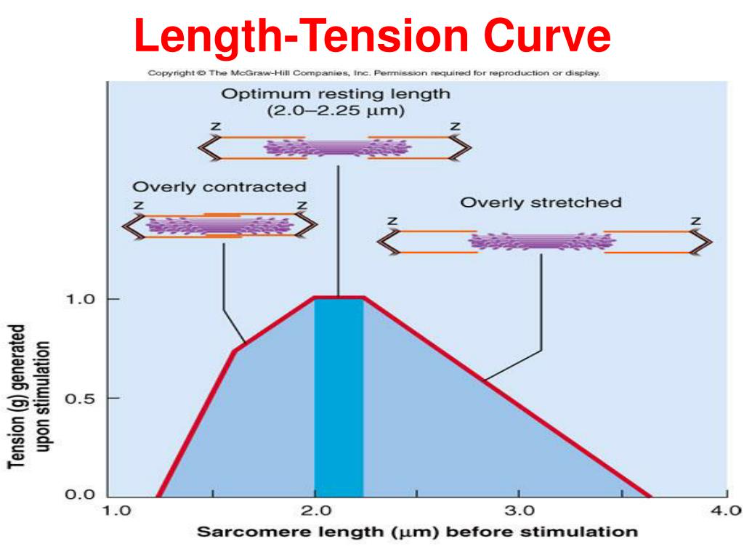
Optimal length-tension relationship of a muscle is the preferred length of the muscle at rest, which in turn allows the muscle to produce the greatest amount of force during movement because there is the ability for sufficient cross bridging of actin-myosin for more significant force generation (Fahmy, 2022). When a muscle is in a shortened and overactive state, the cross bridging of actin and myosin filaments is preestablished in a chronic condition of overlap, which restricts the muscle's ability to generate more force because filament space is limited (Fahmy, 2022). The opposing muscle position is the lengthened and underactive state, which places the actin and myosin filaments apart, thus limiting the cross bridging ability and reducing the capacity to generate force (Fahmy, 2022).
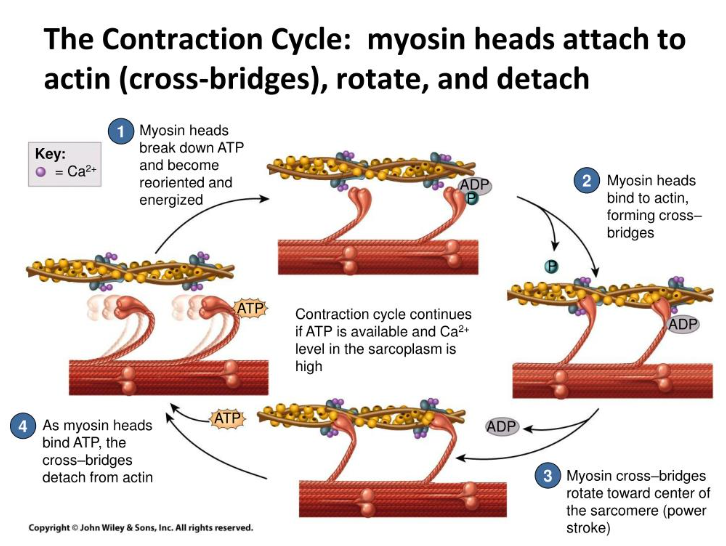
An example of an altered length-tension relationship in the body is when one side of a joint has shortened from overactive musculature resulting in the opposite side of the joint musculature being lengthened and underactive due to decreased neural drive from reciprocal inhibition (Fahmy, 2022). To visualize an altered length-tension relationship in the human musculoskeletal system would be to picture someone who has a rounded shoulder and forward head posture, also known as upper body dysfunction (Brookbush, 2013), which according to Colbert et al. (2022), is possibly due to limitations functional thoracic range of motion causing an incongruent relationship during movement between the thorax convex surface with the scapula concave surface. For more on the structural components, go to https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8811512/. Scroll down to discussion.
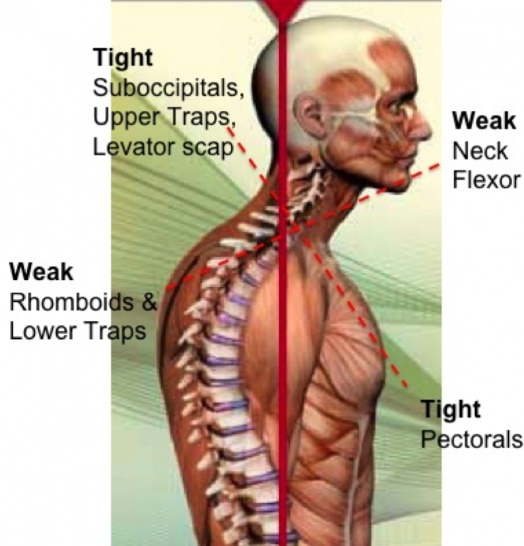
Muscles that stabilize the scapula from the thorax rely on the convex surface of the thorax to maintain an optimal length-tension relationship; such relationships are the serratus anterior, trapezius, and rhomboid (Colbert et al., 2022). Changes in the thorax from a convex to a flatter surface will affect the scapula resting position and inhibit normal movement with the thorax, therefore altering the length-tension relationship of the scapular stabilizers (Colbert et al., 2022). Additionally, muscles affected by the scapulothoracic joint changes and poor posture are the lengthened and underactive upper trapezius, scalenes, sternocleidomastoid (SCM), and rhomboid and the shortened and overactive muscle of the pectoralis major (Colbert et al., 2022). Brookbush (2013) included a detailed list of muscles considered short and overactive based on upper body postural adaptations, which include but are not limited to the pectoralis minor, levator scapulae, latissimus dorsi, teres major, and subscapularis. It's important to note that changes in upper body dysfunction that result in postural adaptations occur gradually over time (Brookbush, 2013). Arthokinematic changes from upper body dysfunctions will eventually lead to mechanical restrictions that will result in greater modifications when compared to soft tissue restrictions alone (Brookbush, 2013).
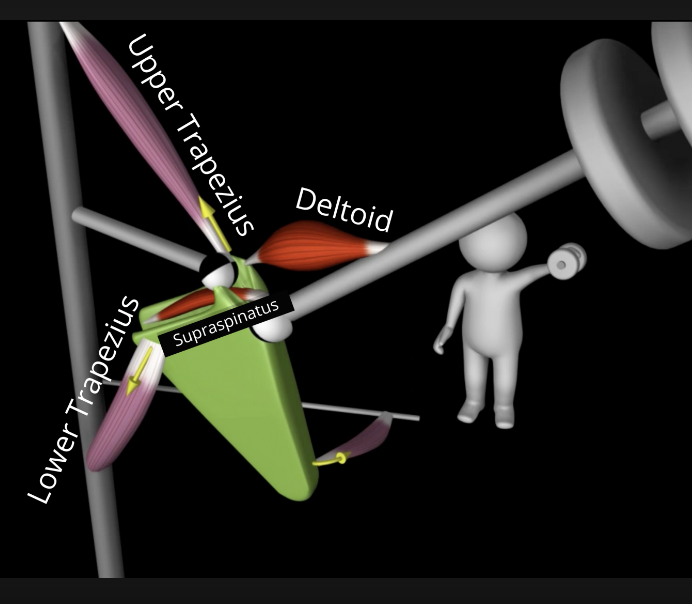
The scapula, in my opinion, is largely a balance of muscles that create force-coupling relationships to maintain adequate alignment of the scapula position with the thorax and shoulder. During shoulder elevation, the scapulothoracic muscles (trapezius, serratus anterior, pectoralis minor, levator scapula, and rhomboid) regulate the scapular movements (Umehara et al., 2019). For the scapula to move optimally, the trapezius and serratus anterior muscles need to function in coordination with the scapulothoracic muscles as a force-coupling relationship (Umehara et al., 2019). The force-coupling relationship between the scapulothoracic muscles is required for optimal scapular and glenohumeral movements (Umehara et al., 2019). An example of a healthy shoulder joint kinematics is elevation, upward and internal rotation, and posterior tilt of the scapula, which means the muscles are working together to maintain force-coupling relationships. When the muscles of the scapulothoracic present with an altered length-tension relationship, such as an underactive and lengthened upper and lower trapezius and serratus anterior with an overactive and shortened pectoralis minor, levator scapulae, and rhomboid the force coupling relationship is decreased, which limits the amount of group force transmitted to the scapula for movement (Umehara et al., 2019). Another way to look at it is the synergy of the muscle groups acting at the scapula is lost due to the imbalances between the muscle groups (Fahmy, 2022).
Article by Denise Fisher 4/5/2023
References
Brookbush, B. (2013). Upper body dysfunction (UBD). Brookbush institute human movement science. Retrieved May 18, 2022, from https://brookbushinstitute.com/course/upper-body-dysfunction-ubd
Colbert, L., Harrison, C., & Nuelle, C. (2022). Rehabilitation in overhead athletes with thoracic outlet syndrome. Arthroscopy, Sports Medicine, and Rehabilitation, 4(1), e181–e188. https://doi.org/10.1016/j.asmr.2021.11.007
Fahmy, R. (Ed.). (2022). NASM essentials of corrective exercise training (2nd ed.). Jones & Barlett Learning.
Umehara, J., Yagi, M., Hirono, T., Komamura, T., Nishishita, S., & Ichihashi, N. (2019). Relationship between scapular initial position and scapular movement during dynamic motions. PLOS ONE, 14(12), e0227313. https://doi.org/10.1371/journal.pone.0227313
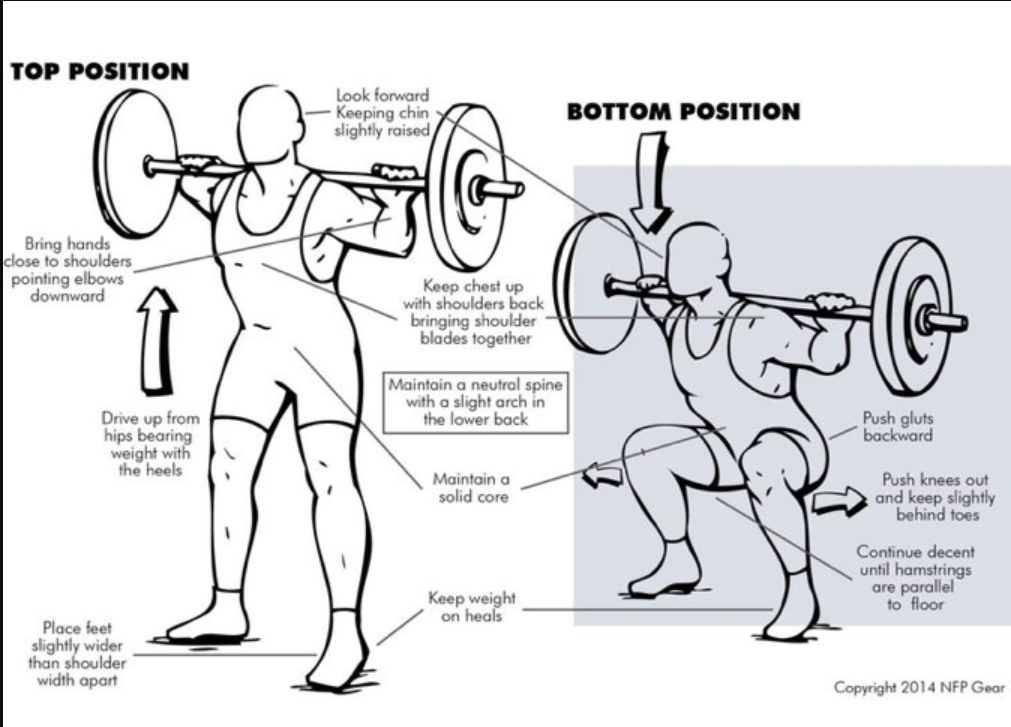
Part 1: Basic Mechanics of the Back Squat
The back squat is a fundamental exercise used in our daily lives and during most resistance training programs; however, it is typically done incorrectly. Squat biomechanics may seem easy, yet it is a complex movement that requires our muscles to coordinate by activating and firing jointly to achieve proper movement patterns. With regard to performance, the back squat is used to improve strength and performance and decrease the risk of injury (Swinton et al., 2012). One such way the back squat reduces injury is by minimizing anterior displacement of the knee (Swinton et al., 2012), which lowers the risk of anterior cruciate ligament (ACL) tears. However, this is only achievable if the squat is done correctly. The figure below is an excellent illustration of what is required to achieve an ideal back squat. Now, it's important to note that there are squat variations, and the image of the back squat below is just an example of the significant components one should achieve while performing the back squat. One feature that was not illustrated and is essential to perform at the feet is to try "spreading the floor underneath your feet." This component should be done throughout the squat movement; the individual will feel more stable when done correctly.
Back Squat Positioning and Additional Considerations
No-heeled shoes. Preferably flat-sole tennis shoes or go without shoes. Heeled shoes make the back squat quadricep-dominant. Quadricep dominant exercises increase ACL loading and anterior shear force.
Stance position will depend on the individual's goals but is primarily related to one's femoral length (thigh bone). A long femoral length requires a wider stance, while a short one needs a more narrow stance. It's also important to understand that an externally rotated foot position will engage the quadriceps more, and a neutral (straight) foot position will engage the tensor fascia lata, IT band, and gluteus medius.
Look slightly upwards the entire time—chest up.
Squeeze shoulder blades and point elbows down.
Spread the floor underneath your feet. Try to tear the floor with your feet.
Lead with the glutes (butt) 1 inch: push the butt back without leaning forward.
Push out with your knees and go down as far as possible.
These considerations aim to spread the pressure out over the entire body. Avoid making one muscle group do all the work, leading to injury.
Figure 1: Back Squat Mechanics
References
Swinton, P. A., Lloyd, R., Keogh, J. L., Agouris, I., & Stewart, A. D. (2012). A biomechanical comparison of the traditional squat, powerlifting squat, and box squat. Journal of Strength and Conditioning Research, 26(7), 1805–1816. https://doi.org/10.1519/jsc.0b013e3182577067
Article by Denise Fisher 3/23/2023